Harbin Institute of Technology News (Sheng Ming Text/Picture) On August 14th, the latest research results of COVID-19, researched by Professor Huang Zhiwei's team, was published online in the journal Signal Transduction and Targeted Therapy with the title of "Adaptive immune responses to SARS-CoV-2 infection in severe versus mild individuals".
As of June 2020, due to the epidemic caused by SARS-CoV-2 had affected more than 8 million people globally. To investigate the mechanism of adaptive immune response to SARS-CoV-2 infection in COVID-19 patients and the establishment of immune memory in rehabilitative patients, the team first applied high throughput sequencing data from single-cell transcriptome and immunological group (TCR/BCR). At the same time, the response mechanism of adaptive immune cells in peripheral blood of COVID-19 patients with different disease severity (severe and mild) was studied in combination with functional experiment. It revealed the immune repertoire reconstruction characteristics of T/B cells in response to SARS-CoV-2 infection and the compositional characteristics of lymphocyte subsets in peripheral blood induced by COVID-19. It was found that the immune memory of T cells and humoral immune response of B cells were closely related to the severity of the disease with a positive correlation. The different immunological characteristics of severe and mild patients was found as well (Fig. 1).
Firstly, the study found that, compared to healthy people, the proportion of COVID-19 patients’ expression cell cytotoxic molecules (such as GZMA, GZMB, PRF1, NKG7) killer T cell subsets (CD8+ effector memory cells (CD8+ TEM), and the CD8+ TEM cell subsets expressing CD45RA(CD8+ TTE) and CD4+ TTE) increased, indicating that the proliferation of these killer T cells is related to COVID-19. At the same time, it was found that the mucosal-associated invariant T cell (MAIT) in COVID-19 patients were significantly decreased; while the consumption of Gamma/delta T cells induced by SARS-CoV-2 has been restored to a certain extent in convalescent patients, but has not yet fully recovered to normal levels. These results indicate that the adaptive immune system of COVID-19 patients is not fully recovered in the early stage.
In order to identify SARS-CoV-2 specific T cell subsets of convalescent patients with COVID-19, the team first studied the clonal expansion of different T cell subsets through scRNA-seq and scTCR-seq, and found that the main T cell subsets responding to SARS-CoV-2 include CD8+TEM, CD8+TTE and CD4+TTE. For the purpose of studying whether these cloned expansion T cell subsets target the SARS-CoV-2, 276 potential T cell epitope polypeptides from the SARS-CoV-2 were used to stimulate the T cells of mild and severe patients, and the reactivity of cells was tested. It was found that there were specific memory T cells of SARS-CoV-2 proteins in convalescent patients with COVID-19, including targeting S protein, and it was found that samples from severe patients showed stronger specific T cell responses, indicating that compared with mild patients, memory T cell reactivity of severe patients to SARS-CoV-2 is stronger.
In terms of B cell immune response, by integrating B cell transcriptome and BCR immune group sequencing data, it is found that BCR clonal expansion is more obvious in severe patients, and the proportion of plasma cells is higher than that of normal people and mild patients. In addition, the immune pathway and complement activation pathway mediated by B cells are up-regulated. These results indicate that a stronger humoral immune response is a typical feature of severe patients.
To further evaluate the recovery of the adaptive immune system of early rehabilitation patients, it was found that no obvious expression of pro-inflammatory cytokines was detected in most of the T/B cells of all recovered patients, indicating that pro-inflammatory cytokines in early convalescent patients with COVID-19 may have returned to normal levels. It is worth noting that the expression of mitogen-activated protein kinase (MAPK) pathways (FOS, JUN, JUNB, and DUSP1) are suppressed in all convalescent patients with COVID-19, which is also consistent with the findings of previous reports.
In addition, this study also found that there is great heterogeneity in the antiviral response of different COVID-19 patients, and it also suggests the possibility that different individuals have different antiviral response mechanisms, which will provide more possibility for subsequent larger-scale cohort studies. For example, many studies have shown that type I and type III interferon (IFN) signaling pathways play an important role in SARS-CoV-2 or SARS-CoV infection, while in this study, The heterogeneity of this IFN response indicates that the relationship of activation of T cell IFN pathway during SARS-CoV-2 infection and its clinical phenotype and antiviral immune response still need to be further elucidated. In a young severe patient (44 years old) case, a high degree of expansion of the IGHV4-34 BCR clone was also found. This clonotype rarely appears in the IgG memory B cells of healthy individuals, and studies have shown that it is related to some autoimmune diseases, suggesting that the autoimmune response induced by viral infection may also be a possible cause of the severe phenotype.
This research is of great significance for understanding the pathogenesis and recovery mechanisms of severe and mild patients, as well as designing vaccines and therapeutic drugs to prevent and treat SARS-CoV-2 infection.
Professor Huang Zhiwei is the corresponding author of the research paper. Associate Professor Zhang Fan, Master student Gan Rui, Doctoral student Zhen Ziqi of the School of Life Sciences and Hu Xiaoli, the Heilongjiang Provincial Hospital Infectious Disease Director are the co-first authors of the research paper. Doctoral students Li Xiang and Zhou Fengxia had made important contribution to this research. This research was funded by the National Natural Science Foundation of China, the Harbin Institute of Technology Young Scientist Studio, and the Harbin Institute of Technology COVID-19 Epidemic Emergency Research Project.
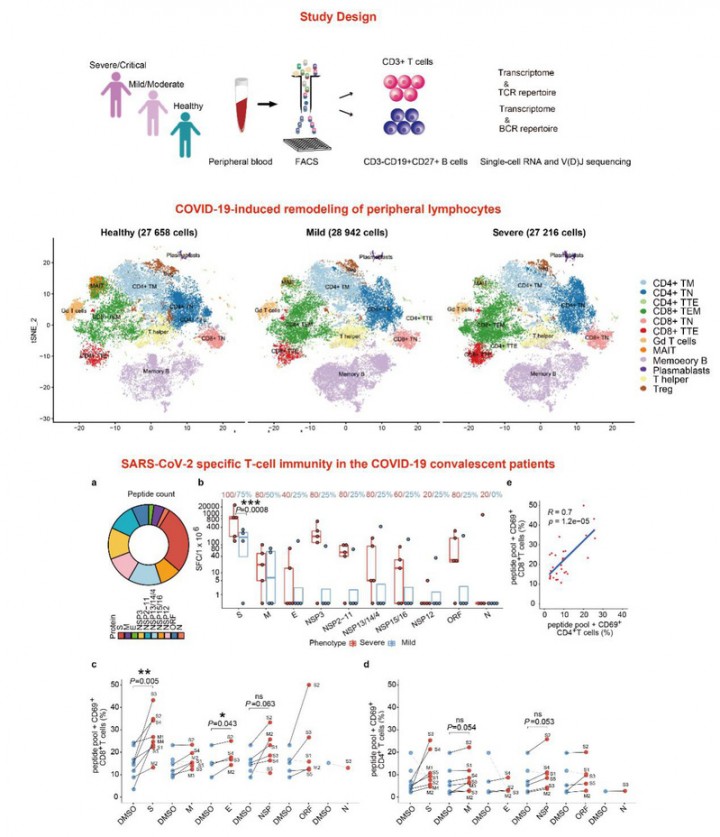
Figure.1 The adaptive immune response and immune memory establishment of COVID-19 patients against SARS-CoV-2 infection